Vitamin D is one of the most talked-about nutrients of modern times – and for good reason. Not only does it affect the bones, as we have long believed, but it has been shown to play a crucial role in everything from the immune system to mood, hormone balance and healthy ageing.
As new research reveals its wide range of effects, awareness of the prevalence of vitamin D deficiency is also growing, especially in northern countries like Sweden.
But what does vitamin D actually do in the body? What are the optimal levels for health and well-being? And how do we get enough – especially during the dark winter months when the sun is absent? In this article, we look at the functions of vitamin D in the body, what the research says about dosing, and how to optimize levels through diet, sunshine and possible supplements.
The role of vitamin D in the body
Vitamin D is not actually a vitamin in the classical sense, but rather acts as a prohormone – a substance that the body converts into a hormone-like active substance. The active form, called calcitriol (1,25-dihydroxycholecalciferol), affects gene expression in hundreds of different cell types in the body(1).
Bone health and mineral balance
Vitamin D is best known for its role in regulating calcium and phosphate levels in the blood. It increases the absorption of these minerals in the gut and ensures that enough calcium is available to build and maintain bones and teeth. Vitamin D deficiency can lead to osteoporosis in adults and rickets in children.
Immune system and inflammation
One of the most exciting areas of research on vitamin D concerns the immune system. Vitamin D has been shown to activate certain immune cells, such as T cells and macrophages, and help the body defend itself against infections. It also has anti-inflammatory properties and is thought to reduce the risk of autoimmune diseases such as MS, type 1 diabetes and rheumatoid arthritis.
Mental health and brain function
Several studies show links between low vitamin D levels and moodiness, depression and cognitive impairment. Vitamin D receptors are found in areas of the brain linked to mood regulation, and deficiency has been linked to both depression and neurodegenerative diseases such as Alzheimer’s.
Hormones, fertility and metabolism
Vitamin D is also involved in hormonal regulation and can affect insulin secretion, thyroid balance and sex hormones. There are indications that adequate levels may promote fertility and reduce the risk of metabolic diseases such as type 2 diabetes.
Muscles, heart and vessels
Vitamin D affects muscle strength and function, and deficiency can lead to muscle weakness and increased risk of falls. It also affects blood pressure regulation and has been shown to play a protective role against cardiovascular disease, although research here is still somewhat mixed.
Longevity – healthy ageing
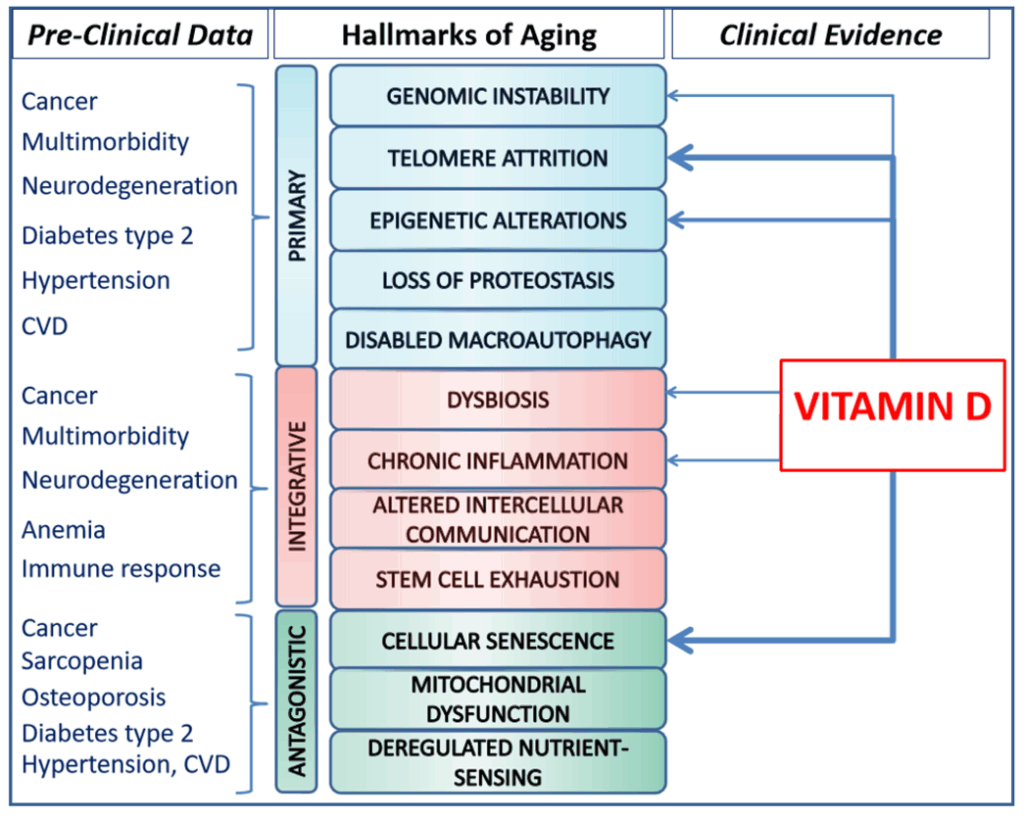
The concept of ‘hallmarks of aging ‘ was introduced in 2013 in a seminal scientific paper by López-Otín et al. published in the prestigious journal Cell(2) to describe the key biological mechanisms driving aging and age-related diseases. First, nine ‘hallmarks’ were presented, which have since been expanded to twelve.
They consist of 12 processes that together explain how the body loses its structural and functional integrity over time. These include genomic instability, telomere shortening, epigenetic changes, protein quality deterioration, mitochondrial dysfunction, cellular senescence and chronic inflammation, among others.
Recent research reviews, including a major review published in 2024 in Nutrients, (3) show that vitamin D also affects several of these key ageing processes at the cellular level.
The study shows that vitamin D acts as a potential longevity modulator by
- Protecting DNA and cells from damage
- Counteracting epigenetic aging
- Improve mitochondrial function, protein quality and gut flora
- Reducing chronic inflammation and cellular senescence
- Supporting stem cell function and immune balance
These effects occur both through hormone-like signaling via vitamin D receptors (VDRs) and through gene regulation in the cell nucleus.
Optimal levels of vitamin D in the body?
When people talk about ‘measuring vitamin D in the blood’, they are not actually referring to the vitamin D itself, which comes from the sun or diet, but to 25-hydroxyvitamin D, also known as 25(OH)D. This is the form of vitamin D that circulates longest in the blood and is therefore the most reliable marker of the body’s vitamin D status.
Vitamin D undergoes two conversion steps in the body:
- First, vitamin D (from the sun or diet) is converted in the liver to 25-hydroxyvitamin D – this is the form measured in blood tests.
- Then 25(OH)D is further converted in the kidneys (and in some other tissues) to the active form, 1,25-dihydroxyvitamin D (calcitriol), which exerts hormone-like effects in cells.
Although calcitriol is the most active form, it is 25(OH)D that is used in blood tests because its levels reflect the body’s vitamin D stores over time. This is because calcitriol can be normal even when deficient, as the body can compensate temporarily – therefore it does not give a true picture of total vitamin D stores.
Recommended levels
According to the Swedish National Food Agency, the threshold for adequate levels is ≥50 nmol/L, while deficiency is defined as below 25 nmol/L. However, functional medicine and international guidelines often set a more ambitious target. Many functional medicine physicians and nutritionists recommend aiming for levels of 75-125 nmol/L, especially in cases of autoimmunity, chronic fatigue or depressive disorders.
Risk groups for shortages
Several groups are at increased risk of developing vitamin D deficiency:
- Older people – the skin loses its ability to produce vitamin D with age.
- People with dark skin – higher melanin reduces vitamin D synthesis from the sun.
- Those who wear full-length clothing or spend a lot of time indoors – less sun exposure.
- Living in northern countries – from October to April, UVB radiation is insufficient to form vitamin D in the skin.
- Overweight or obese people – vitamin D is stored in fat tissue and becomes less available.
- Individuals with impaired bowel function – e.g. celiac disease, Crohn’s disease or IBS, where absorption may be impaired.
Blood samples can be taken through the health center or as a self-test through various health companies. It is important that the sample is analyzed in a reliable lab. Note that high levels are not always better.
Can you get too much vitamin D?
Although vitamin D deficiency is much more common, it is quite possible to get too high levels with excessive intake of supplements. The body has natural protection against overproduction from sun exposure, but this does not apply when taking large amounts of vitamin D in tablet form.
Long-term blood levels above 150-200 nmol/L increase the risk of hypercalcemia – a condition where calcium levels in the blood become too high. This in turn can lead to:
- Nausea and fatigue
- Kidney problems (e.g. kidney stones or kidney failure)
- Cardiac arrhythmias
- Calcium deposition in soft tissues (blood vessels, kidneys, lungs)
Toxic levels usually require very high daily doses (e.g. >10,000 IU/day for a long time), but individual sensitivities vary.
Vitamin D and vitamin K2 – an important combination
When taking vitamin D in supplement form, especially in doses above 2 000 IU/day, it is wise to combine it with vitamin K2 – a vitamin that plays a key role in calcium metabolism.
While vitamin D increases the absorption of calcium from the gut, K2 helps to direct this calcium to the right place – the bones and teeth – and away from the wrong place – such as blood vessels and soft tissues.
K2 activates the protein osteocalcin (for storage in bone tissue) and Matrix GLA protein (which inhibits calcification in the vessel walls). Without sufficient K2, there is a risk that high vitamin D levels may contribute to vascular calcification in some individuals.
Summary:
- Always combine vitamin D supplements with K2 – especially for long-term intake.
- Choose a supplement that contains both, or take them separately but in parallel.
- The MK-7 form of K2 is the most long-acting and well-studied.
How do you get vitamin D?
Vitamin D is unique among vitamins in that the body can produce it in significant and sometimes sufficient quantities itself – but only under the right conditions. In Sweden, there is not enough sunlight all year round, so it is important to also look at diet and possible supplements.
Sunlight – the most important natural source
When the skin is exposed to UVB radiation from the sun, cholesterol in the skin is converted into vitamin D (cholecalciferol). However, several factors influence how much vitamin D we actually produce:
- Latitude: In Sweden, we produce almost no vitamin D between October and April, because the sun is too low.
- Time of day: Maximum production occurs between 10 and 15 am when the sun is high.
- Skin type: The darker the skin color, the more melanin – and the more UVB blockage.
- Clothing and sunscreen: Protects against burns – but also blocks vitamin D synthesis.
- Age: Older people have less ability to produce vitamin D in their skin.
About 15-30 minutes of midday exposure to the face, arms and legs, a few times a week during the summer months, can be enough to replenish the body’s stores – provided the skin is bare and without sunscreen.
Dietary vitamin D
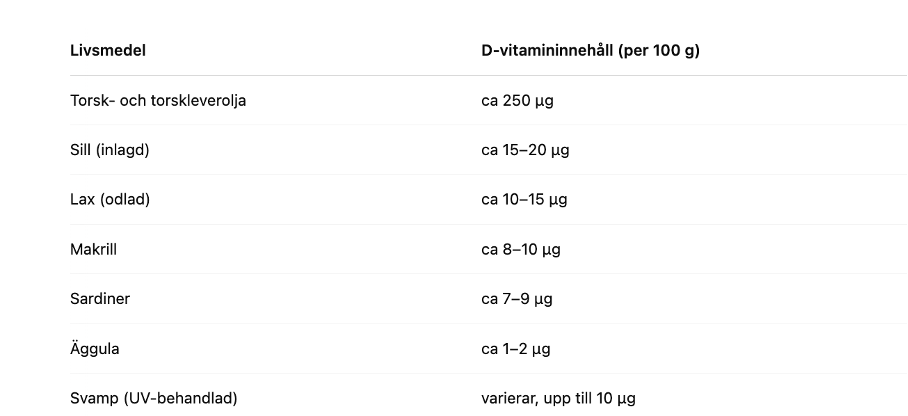
Although the body can produce vitamin D itself through sun exposure, dietary intake is an important source – especially during the winter months in northern countries where UVB radiation is insufficient.
Most natural sources of vitamin D come from animal foods, especially from the sea. Oily fish is the most concentrated source of vitamin D in the regular diet.
Calculate your individual need for vitamin D supplementation
To achieve optimal levels of vitamin D in your blood, it can be helpful to calculate how much extra vitamin D you need. According to a formula used in clinical practice, you can estimate your daily supplementation needs as follows:(4)
Total requirement in IU = 39.7 x (target level in nmol/L – current level in nmol/L) x body weight in kg
The formula gives the total amount of vitamin D in IU (International Units) needed to raise 25(OH)D to a desired level.
The formula is based on the assumption that 50% of vitamin D intake is actually absorbed and used by the body. In otherwise healthy people, about 50-70% absorption is considered normal. However, in the presence of certain risk factors (obesity, intestinal problems, old age), absorption can drop to 30-50%.
Example
If your current level is 50 nmol/L and you are aiming for 100 nmol/L and weigh 65 kg:
Total need in IU = 39.7 x (100-50) x 65 = 129 025 IU
Per day for 60 days = 2 150 IU
Dividing this dose over 60-90 days is a common way to avoid rapid peaks in blood levels and reduce the risk of side effects such as hypercalcemia. It gives the body time to slowly replenish its vitamin D stores.
Vitamin D is replenished gradually and stored in fat tissue. In some cases, a higher initial dose (known as a loading dose) may be needed for 1-2 weeks in case of severe deficiency, but this should always be done in consultation with your healthcare provider.
Please note: This formula is an estimate and individual factors such as age, skin color, sun exposure and gut health may affect the need. It is therefore important to follow up with regular blood tests and consult with a healthcare provider to adjust the dosage if necessary.
Summer – your natural chance to replenish your vitamin D stores
In Sweden, summer is our main chance to replenish our body’s vitamin D stores naturally. Between May and September, the sun’s UVB radiation is strong enough for the skin to effectively produce vitamin D – something that is not possible during the winter months at our latitudes.
By spending regular time outdoors in the middle of the day, roughly between 10 a.m. and 3 p.m., and exposing the face, arms and legs for 15-30 minutes a few times a week, the body can store sufficient amounts of vitamin D to cover much of its winter needs. However, it is important to avoid burning the skin, as overexposure does not increase vitamin D production but can damage the skin in other ways.
Vitamin D is fat-soluble and can be stored in the body’s fat tissue and liver. With good sun exposure during the summer, these stores can last for about three to four months, but then levels gradually start to fall during the fall and winter.
It is therefore wise to measure your 25(OH)D levels in early October to see how well the summer has replenished stocks, and again in late January or February to identify if levels have become too low. If the October blood test shows levels below 75 nmol/L, or if you belong to a risk group such as the elderly, people with darker skin tones or those who spend a lot of time indoors, it may be advisable to start vitamin D supplementation in early fall.
Harnessing the sun’s free resource during the summer – in a wise and balanced way – is one of the most effective and natural ways to support immune function, brain health, muscle strength and long-term vitality. Your health starts in the summer sun.
References
- Vitamin D: Evidence-Based Health Benefits and Recommendations for Population Guidelines
- Hallmarks of aging: An expanding universe, published in Cell 2022
- Targeting the Hallmarks of Aging with Vitamin D: Starting to Decode the Myth, published in Nutrients 2024.
- Cholecalciferol loading dose guideline for vitamin D-deficient adults, Europena Journal of Endocrinology 2010