The gut-brain axis acts as a complex and bidirectional communication pathway connecting the gastrointestinal tract to the brain. It manages information flows through neurons, hormones and the immune system, with the gut microbiota playing a central role. More recently, research is beginning to investigate how frequencies, such as electromagnetism in the form of light, sound and vibration, affect this important axis.
Different parts of the gut-brain axis
Enteric nervous system and vagus nerve
The stomach and intestines house the enteric nervous system (ENS), often called the ‘brain of the gut’. This extensive network of neurons extends from the esophagus to the rectum and functions independently, but also actively communicates with the brain via the vagus nerve – a key link in the gut-brain axis.
The endocrine system
In addition to neural signaling pathways, the endocrine system contributes crucial hormones such as cortisol (stress), ghrelin (hunger) and serotonin. Interestingly, the gut produces about 90% of the body’s serotonin, which is important for bowel movements, digestion and immune system functions. Through the vagus nerve and gut microbiota signals, the brain’s serotonin levels are also affected, which in turn influence mood, emotional balance and cognitive abilities.
The immune system and the microbiota
In addition, the immune system is a key player, as much of the body’s defenses are located in the intestinal tissue, including the mucosa and parts of the lymphatic system. When the gut flora becomes imbalanced, inflammatory processes are triggered that affect the whole body, including the brain. Inflammation in the brain can contribute to neurological and psychological problems(1).
In addition, the gut is home to trillions of microorganisms – the microbiota – that directly influence brain chemistry by producing neurotransmitters such as dopamine (motivation), GABA (calmness) and short-chain fatty acids (SCFAs). These fatty acids, formed when gut bacteria ferment dietary fiber, maintain the gut barrier, reduce inflammation and improve energy use by brain cells(2).
The gut-brain axis is thus a sophisticated and integrated system. The gut not only responds locally to diet, but is also affected by your emotional and mental health. A disruption in this axis can result in nutritional deficiencies, gastrointestinal problems, autoimmunity, anxiety and depression.
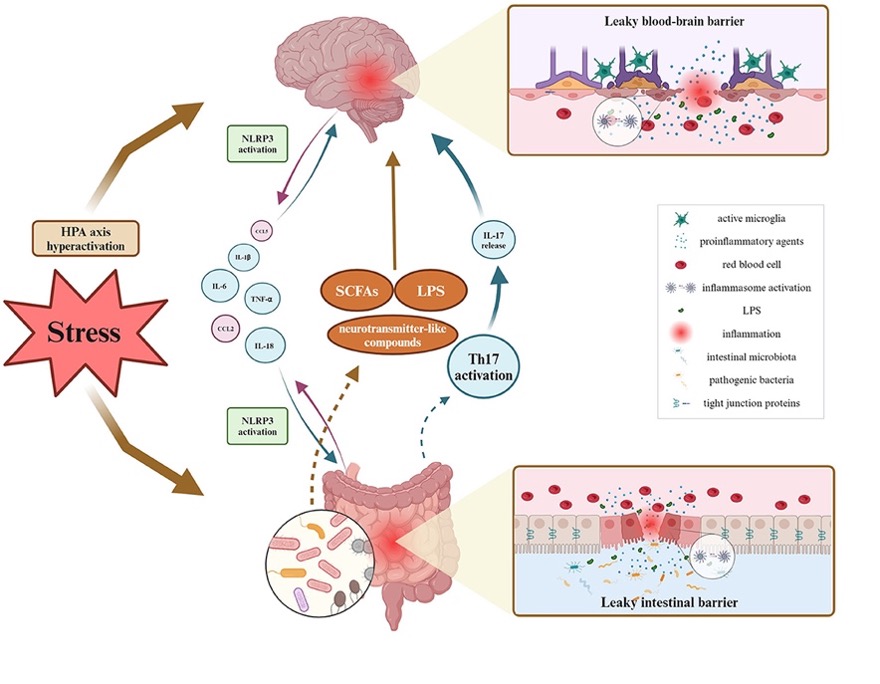
The impact of stress on the gut-brain axis
Stress strongly affects the gut-brain axis by activating the sympathetic nervous system (“fight-or-flight”), causing several negative effects on digestion(3)
- Reduced stomach acid production: Stress reduces the release of hydrochloric acid (HCl) in the stomach, making the breakdown of proteins more difficult and impairing nutrient absorption. This often leads to bloating, acid reflux and weaker gut flora.
- Reduced enzyme production and bile flow: Stress inhibits the pancreas’ secretion of digestive enzymes, making it harder to break down food. At the same time, bile flow is impaired, which can cause problems with fat breakdown and increase the risk of gallstones.
- Altered bowel motility: Stress can speed up bowel movements and cause diarrhea, or slow them down and contribute to constipation.
- Increased gut permeability – ‘leaky gut’: Cortisol, the body’s primary stress hormone, damages the gut mucosal barrier, allowing harmful substances to enter the bloodstream and trigger inflammation. Research shows that a permeable gut barrier also affects the blood-brain barrier in the same way, leading to ‘leaky brain’. This releases inflammatory molecules and toxins that travel through the blood to the brain and cause inflammation. An inflamed brain can cause symptoms such as brain fog, anxiety and neurodegenerative diseases such as Alzheimer’s.
- Weaker vagus nerve: Stress reduces vagus nerve activity, which impairs communication within the gut-brain axis. Low vagal tone is linked to IBS, inflammation and poor digestion.
- Gut flora imbalance: Stress disrupts the balance of gut flora and reduces levels of beneficial bacteria, affecting neurotransmitters such as serotonin, GABA and dopamine – important for mood, stress management and cognitive functions.
How can we optimize the gut-brain axis?
You can improve the gut-brain axis yourself by balancing the microbiota, reducing inflammation and supporting nervous system health. Here are the most effective strategies.
The role of diet in the gut-brain axis
Optimizing the diet strengthens both gut flora and brain health. By including the right nutrients, you balance the microbiota and improve brain function. A high-fiber diet, especially prebiotics from vegetables, berries, nuts and root vegetables, nourishes gut bacteria and contributes to a healthy microbiota, while reducing inflammation in the body.
To further strengthen the gut flora, fermented foods such as kimchi, sauerkraut, kefir and yogurt are excellent. They provide probiotics, increase the diversity of good bacteria and stimulate the production of serotonin and GABA, which positively affect mood and stress levels. In addition, polyphenols – found in colorful plants such as berries, fruits, vegetables, coffee, tea and dark chocolate – provide antioxidants that support both gut flora and brain function.
Specific Nutrients for the gut-brain axis
Omega-3 fatty acids, found in oily fish, flaxseeds and walnuts, have an anti-inflammatory effect and reduce neuroinflammation, improving brain health. Extra virgin olive oil (EVOO) acts as a powerful boost for the gut-brain axis thanks to its polyphenols and monounsaturated fats. Oleic acid (omega-9) supports brain plasticity, nerve signaling and protects against neuroinflammation, while strengthening the vagus nerve.
Amino acids also play an important role. Tryptophan, found in turkey, eggs and pumpkin seeds, is converted into serotonin and improves both mood and sleep quality. Tyrosine, found in avocados and chicken, contributes to dopamine production and boosts motivation and concentration.
Stress management
The vagus nerve plays a central role in the body’s stress regulation and digestion and can be stimulated through deep breathing, meditation, cold baths and singing, among others. Any practice that activates the parasympathetic nervous system and lowers stress levels improves digestion and supports a balanced microbiota.(4)
Adaptogens such as ashwagandha, rhodiola and holy basil have been shown to help the body adapt to stress by regulating cortisol levels.
Regular mindfulness and meditation have been linked in studies to improved gut flora and reduced inflammation, which in turn can positively affect both mood and the immune system.
To further support the body’s natural calming system, foods rich in GABA, such as green leafy vegetables, kimchi and magnesium-rich foods, can contribute to increased relaxation, improved sleep and a more balanced gut-brain axis.
Sleep optimization for the gut-brain axis
Stable and restorative sleep strengthens both the brain and the gut flora, as the circadian rhythm affects the balance and function of the microbiota. By keeping a regular sleeping and waking time, you synchronize the body’s circadian rhythm with the work of the gut.
As blue light in the evening can inhibit melatonin production, it helps to use blue light filters on screens or wear blue light blocking glasses. Melatonin not only regulates sleep, but also positively affects the composition and function of the intestinal flora.
To further support sleep, magnesium and glycine can be beneficial. Magnesium calms the nervous system and reduces stress, while glycine improves sleep quality by lowering body temperature and promoting deep sleep.
Movement and exercise
Movement and exercise support the gut-brain axis by influencing the nervous system, microbiome and body inflammation levels. Low-intensity exercise, such as walking and yoga, stimulates the vagus nerve and improves digestion and stress management.
Regular movement also balances the autonomic nervous system, which contributes to stable gut motility and healthy gut flora.
High-intensity exercise and fascia stimulation
High-intensity exercise, such as interval and strength training, releases the brain growth factor BDNF, which improves cognitive function, nervous system plasticity and learning ability. This exercise also increases blood circulation, which benefits both the brain and the gut by optimizing oxygen and nutrient uptake.
Stretching and fascia stimulation reduce tension in the gastrointestinal tract and improve digestion. The condition of the fascia affects circulation and the lymphatic system, contributing to better nutrient absorption and a more relaxed intestinal motility.
Avoid what damages the gut-brain axis
To support the gut-brain axis, you need to avoid factors that damage the gut flora, the nervous system and their interaction.
- Ultra-processed foods, which often contain additives, refined oils and sugars, increase inflammation and reduce gut flora diversity, impairing digestion and neurotransmitters such as serotonin.
- Alcohol, sugar and wheat flour weaken the intestinal barrier and contribute to increased intestinal permeability, also known as ‘leaky gut’, this can lead to neuroinflammation and negatively affect brain function.
- Chronic stress directly affects the gut-brain axis by disrupting the balance between serotonin and cortisol. This impairs communication between the gut and the brain, raises inflammation levels and affects mental well-being.
- Another factor potentially damaging to the shoulder is exposure to electromagnetic fields (EMF ) from cell phones, Wi-Fi and other wireless technologies. You can reduce the risk by limiting screen time, especially in the evening, and using airplane mode on your phone at night to reduce EMF exposure.

How frequencies affect the gut-brain axis
A new review study from Cornell University examines how sound, light and vibration affect the gut-brain axis and microbial ecosystems.(5) The body’s microbiota functions as part of a global network of microorganisms, called the “Internet of Microbes”.
Within this network, microbes communicate via electromagnetic signals, sound vibrations and light waves, affecting the body’s biological processes. By understanding these signals, we can find new ways to balance gut flora, support health and even influence the environment around us.
This communication relies on biophysical and electromagnetic processes, with microbes responding to their environment through signals that propagate both locally and over distance. Scientists are now exploring how we can use these interactions to improve the gut-brain axis and promote sustainability in both body and ecosystem.
Sound and the gut-brain axis
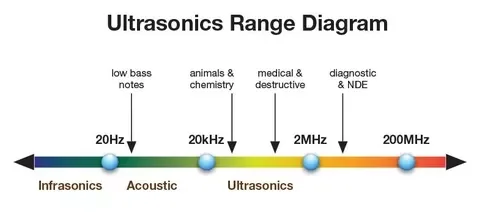
Sound affects the gut-brain axis more than you might think. It controls bacterial growth, metabolism and communication. Microbial communities use sound vibrations to transmit signals and adjust their biochemical activity, meaning that different sound frequencies directly affect both the gut flora and the nervous system.
- Low frequencies (0.1-20 Hz), infrasound, are frequencies that humans cannot hear but that some animals such as whales and elephants can hear. These affect the metabolism of bacteria and stimulate the vagus nerve – an important link in the gut-brain axis. By calming the nervous system, they reduce inflammation.
- Mid-range frequencies (20 Hz-20 kHz) can be heard by humans and range from deep bass to high notes like birdsong. These frequencies help bacteria form protective biofilms, which support gut health. Some music frequencies, such as 432 Hz and 528 Hz, are linked to relaxation and better cell communication.
- Ultrasound (>20 kHz) is above human hearing but can be heard by many animals such as dogs and bats. These frequencies are used in medicine to affect cells, microbiota and the nervous system. It also stimulates digestion and certain biological processes in the body.
On the other hand, research shows that constant exposure to noise and white noise disrupts gut flora and increases inflammation. White noise, which consists of all audible frequencies in equal intensity, is similar to a static background tone – like a fan or a TV without a signal. Although it is sometimes used to improve sleep, too much exposure can negatively affect the nervous system in ways we do not yet fully understand.
Light and the gut-brain axis
Light regulates circadian rhythms and the immune system, but also affects the microbiome and brain health through the gut-brain axis.
- Infrared light (700-1100 nm) cannot be seen with the naked eye. It is found in sunlight and in fire and embers. Some frequencies of IR light can also generate heat. This light stimulates the mitochondria of cells, increasing energy production and reducing inflammation. Wavelengths of 810-850 nm strengthen the vagus nerve and improve communication in the gut-brain axis.
- Red light (600-700 nm) is visible. It does not penetrate as deeply into the body as infrared light but has a positive effect on cell functions, especially skin and blood circulation.
- Blue light (400-480 nm) is an important part of the visible light spectrum and has a strong effect on circadian rhythms, hormones and neurological functions. Overexposure in the evening disrupts the circadian rhythm and negatively affects the gut-brain axis.
- Ultraviolet light (UVB, 280-315 nm) is invisible to the human eye. It increases vitamin D production, which indirectly supports the gut immune system and microbiome.
The study also shows that constant artificial light can disrupt the microbiome and lead to inflammatory diseases.
Vibrations and the gut-brain axis
Vibrations, especially mechanical and electromagnetic waves, affect the activity of bacteria and the nervous system’s regulation of inflammation and intestinal motility.
- Nanovibrations (0.1-10 Hz): These low-frequency vibrations affect the growth and metabolism of bacteria, which can balance the gut flora and its connection to the brain. Earthing and pulsed electromagnetic fields (PEMF) provide access to these signals. Breathing exercises and meditation also create subtle vibrations that support the gut-brain axis.
- Whole body vibration (20-50 Hz): Used in medicine and exercise to improve nerve signaling and circulation. Vibration plates and tactile stimulation, such as massage guns or TENS, stimulate digestion and bowel movement.
- By stimulating the vagus nerve with mechanical vibrations, we can improve both mental and physical health via the gut-brain axis. Electrical vagus nerve stimulation is used in healthcare and various wearables are available for consumers, such as Pulsetto and Neruosym.
Read more about the electromagnetic spectrum in our previous article on Our charged cells and electromagnetism.
Bioresonance and the gut-brain axis
The study above describes how microorganisms communicate through light, sound and electromagnetic signals – a basis for bioresonance. Metatron, an advanced bioresonance technology, analyzes the body’s quantum frequencies using non-linear analysis (NLS).
Metatron technology reads frequency signatures from tissues and organs, including those associated with the gut flora and nervous system. Microorganisms, cells and organs emit specific electromagnetic frequencies, which can be in balance or out of balance depending on the state of health.
By identifying disturbances, bioresonance diagnostics map imbalances in the microbiome and nervous system. When an imbalance is found, Metatron transmits corrective frequencies to restore balance and stimulate the body’s self-healing.
Frequency-based stimulation of the gut-brain axis and the microbiome opens new possibilities for health and well-being. This axis is influenced by lifestyle, diet, mental state and electromagnetic signals. By understanding these factors, we can develop new approaches to balance the gut flora, optimize the nervous system, and improve both gut health and mental well-being.
As research progresses, it is becoming clearer that frequencies may be the key to supporting the body’s functions. Perhaps the future of medicine lies not in chemicals, but in signals.